At RSNA 2025, Alexander Drzezga, MD, Director of the Department of Nuclear Medicine at the University Hospital Cologne, presented a compelling overview of how advanced imaging is transforming the landscape of Alzheimer’s disease.
Neurodegeneration spans multiple disorders, but as Drzezga noted, “more than half of all cases are due to Alzheimer’s disease.” Prevalence rises dramatically with age, as about 20% of the subjects above the age of 80 are already suffering from Alzheimer’s disease.
With global aging, the number of people living with Alzheimer’s will nearly double by 2050, representing “an enormous burden on the patients, on their families, but also on our social systems.” As he summarized, “So obviously, we need to do something about it.”

Disease-Modifying Therapies and the Imaging Imperative
For the first time, monoclonal antibodies that remove amyloid plaques offer meaningful therapeutic impact. These treatments “slow the clinical decline by about 30%.” Although not curative, “for the first time in history we are able to actually delay the progression of disease significantly.”
This shift amplifies the need for precise biomarkers. Clinical assessment alone is insufficient because “one pathology can cause different clinical pictures, and various pathologies can cause similar clinical pictures.” Imaging – amyloid PET, tau PET, and FDG PET – can directly visualize the three defining features of Alzheimer’s: amyloid deposits, tau tangles, and neurodegeneration.
FDG, Amyloid, and Tau PET: From Diagnosis to Prediction
FDG PET remains a versatile tool revealing characteristic metabolic patterns across Alzheimer’s disease, frontotemporal dementia, and Lewy body dementia.
Amyloid PET adds causal clarity. In atypical presentations such as posterior cortical atrophy or logopenic aphasia, scans can reveal that “all three of them have their brains full of amyloid,” confirming they are “suitable for anti-amyloid treatment.”
Tau PET provides even richer insight. It not only identifies Alzheimer’s pathology but also highlights “the region of the major ongoing neurodegeneration,” making it effectively “a combination of FDG PET and amyloid PET.” Because tau accumulation correlates closely with symptoms, tau PET is “well suitable also for quantitative staging.”
Combined PET biomarkers powerfully improve prognostication. Amyloid-positive patients who are also FDG-abnormal “will convert to dementia in 80% of cases,” while amyloid-positive/FDG-negative individuals often remain stable. In cognitively healthy adults, adding tau PET helps identify those most likely to experience decline, strengthening preventive trial design.
Quantification, Therapy Monitoring, and Emerging Technologies
Standardized quantification like the centiloid scale translates amyloid burden into a 0–100 index. Under therapy, patients can drop by ~80 centiloids; some “actually went amyloid negative.”
MRI remains critical for tracking amyloid-related imaging abnormalities (ARIA), which occur in “20 to 30% of cases.” New antibodies, such as bispecific agents using a transferrin shuttle, may reduce ARIA risk to “below 5%.”
On the therapeutic horizon, anti-tau strategies – including antisense oligonucleotides that “basically block the synthesis of new Tau”– show early promise in reducing tau aggregation.
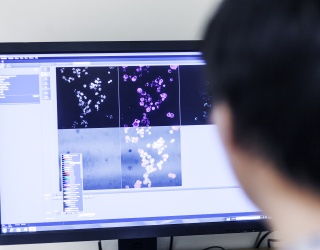
AI innovations are also accelerating progress. Drzezga highlighted a generative model capable of producing a synthetic tau PET from structural MRI, noting the images look “quite strikingly similar.”
Super-Agers and the Biology of Resilience
Research into “super-agers” reveals people over 80 with exceptional cognition whose brains are “free of any tau or amyloid pathology.” Even centenarians show similar resistance. Meanwhile, lifestyle factors such as education play a protective role: individuals with higher education “would tolerate more tau in their brain” before symptoms develop.
The developments presented underline how quickly Alzheimer's diagnostics is changing and how crucial imaging already is for therapy decisions today.