Prostate cancer remains the second most common cancer in men, with 1.5 million new diagnoses and 400,000 deaths each year — numbers projected to rise sharply by 2040. At Bayer’s “Transforming the Future of Prostate Care” event to kick off the European Society of Medical Oncology Congress taking place in Berlin, we spoke with Professor Bernd Hamm, Department of Radiology at Charité Berlin and Dr. Peter Seidensticker, Head of Medical Affairs Radiology at Bayer about how long-term partnerships, clinical insight, and digital transformation are paving the way for more precise and patient-centered care.
Prof. Hamm, please explain your involvement with Bayer. Is it merely a convenience that both you and the organization are based in Berlin, or is there more to it?
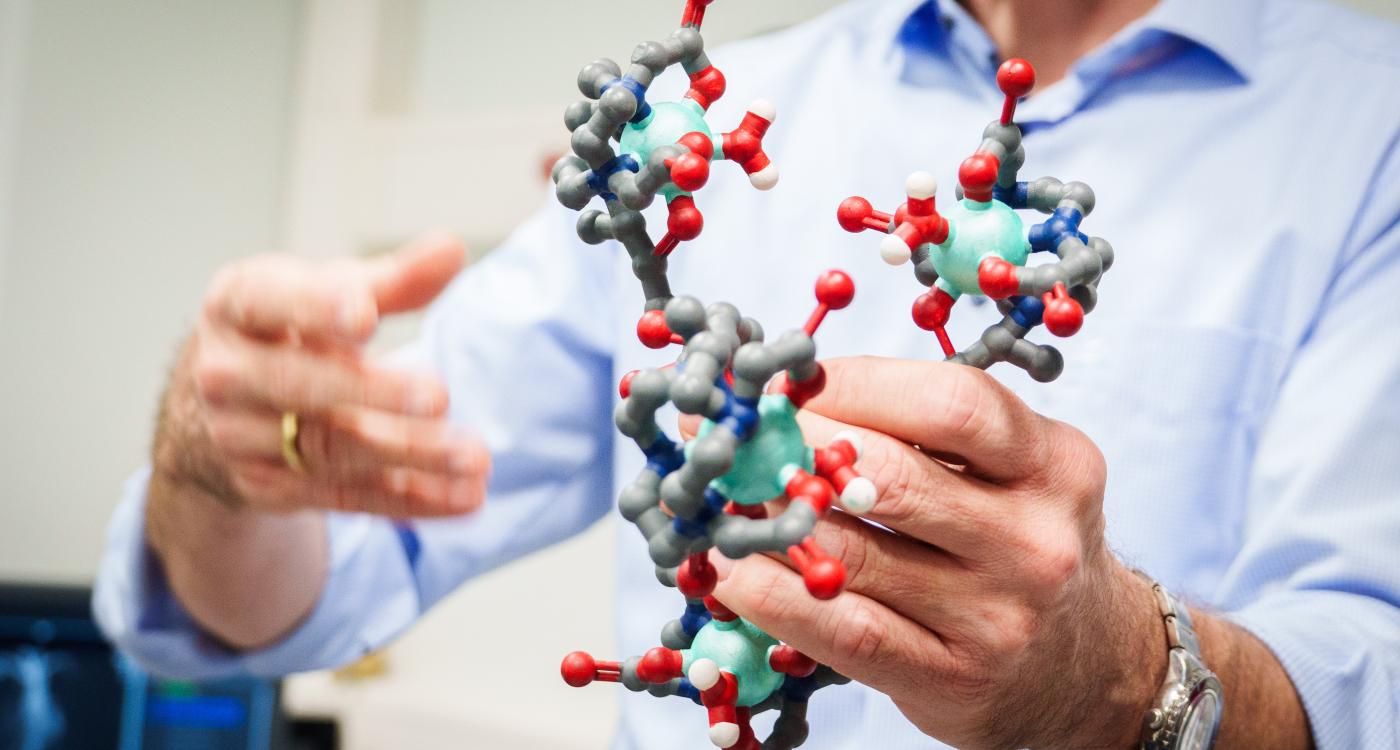
Prof. Hamm: Our cooperation with Bayer has been long-standing, spanning several decades and covering various areas, including the development and clinical testing of contrast media. As Bayer is now focusing on improving therapies for prostate cancer, there is a close collaboration regarding prostate cancer diagnosis. Since both Bayer and Charité are located in Berlin, it was a natural step to cooperate on the PROKOMB trial.
In summary, there is a strong and productive partnership with Bayer, which dates back many years and has its roots in earlier collaborative efforts.

Long-Standing Collaboration Between Bayer and Charité Drives Innovation in Prostate Cancer Imaging
You are here in conjunction with the ESMO Congress. What advances are you seeing in the detection of various cancers through your specialty?
Prof. Hamm: To answer the question in general is becoming more difficult because we now have so many different types of cancers. The more diverse these cancers are, the more challenging and distinct the imaging modalities and approaches become. In some cases, PET-CT might be the best option. For example, in lung cancer, CT works excellently, while MRI is preferred for liver, prostate, or gynecological cancers.
Imaging is becoming increasingly important in oncology, not only for diagnosis but also for monitoring and follow-up. This includes two main aspects: first, assessing the tumor’s response to therapy, since some treatments are very expensive and it’s essential to confirm whether there is a response or not; and second, identifying potential side effects of therapies, not just following up on the tumor itself, but also detecting treatment-related complications.
Specifically, regarding prostate diagnosis, what are the current guidelines for prostate cancer detection and what is the general path for those requiring further investigation all the way up to intervention?
Prof. Hamm: There are established guidelines for the detection of prostate cancer — these are the guidelines of the European Association of Urology, developed in collaboration with other societies. The guidelines recommend starting with PSA testing. If the PSA level is very low, it should be repeated no earlier than every five years. If the PSA value is in the intermediate range, testing should be repeated every two years.
If the PSA level is above three, it is important to check for other possible reasons for the elevated value. If no such reasons can be found, especially in cases where there is a family history of prostate cancer, then an MRI should be performed. This can be either multiparametric (with contrast agent) or biparametric (without contrast agent) to determine whether there is suspicion of clinically significant cancer.
The PI-RADS classification provides an estimate of the likelihood of clinically significant prostate cancer. PI-RADS 3 is considered equivocal, meaning “I don’t know,” while PI-RADS 4 and 5 indicate that prostate cancer is likely or very likely.
According to the European guidelines, PSA testing should start at the age of 45. If there is a family history of prostate cancer or the patient is of African descent, where prevalence is higher, testing may start earlier, at around 40. Importantly, MRI should be performed before proceeding to biopsy.

Dr. Seidensticker, Bayer’s involvement to radiology is, of course, extensive. However, you are also featuring and supporting many aspects of the specialty for which there seems to be no direct commercial justification for your company. What, then, is the motivation behind this commitment?
Dr. Seidensticker: At Bayer, we have always felt a strong commitment to the diagnostic imaging community. Some areas – at first sight maybe not obvious – make an integral part of our partnership with the community, and they play an essential role in our relationships with experts like Professor Hamm and many others.
We aim to lead by example and want to be a valuable partner long-term for the imaging community. This close connection has always been one of the reasons why we have been so effective in driving innovation in this field.
AI, Data Protection, and Digitalization: Balancing Innovation With Regulation in Radiology
Prof. Hamm, in addition to honoring your incredible leadership in research and publication, I also want to get your input on the IT side of radiology, specifically AI in the diagnostic portfolio. Are there current opportunities you feel are being underutilized?
Prof. Hamm: The answer is somewhat specific to Germany. Our data protection regulations are very strict, which means we still write reports on paper and send them by mail. As a state-owned hospital, we are not allowed to send reports by email. I was recently in China, and there everything is digital. The patient receives a code and can download both the images and the report directly using that code.
When we talk about AI, the challenges are essentially the same. The main obstacle is digitalization itself, especially in combination with data protection regulations. Interestingly, although we all share the same data protection framework in Europe, the way it is implemented varies completely. For example, we are participating in a multicenter trial in Spain, and there they say, 'No problem, you can send us the data.' In Germany, that would not be possible.
So, there is a strong need for digitalization, and the data protection law remains a major hurdle.
At the ECR in the past few years, there was a major focus on the acquisition of anonymized patient data for research purposes. Do you have any involvement in that or any information on how it is progressing?
Prof. Hamm: Yes, it is progressing. There is a new law stating that if patient data are collected with the support of a governmental or public grant, then these data belong to the public. You cannot claim ownership and refuse to share them.
So, if the data are collected with public funding, you are required to make them available to other researchers, which is reasonable. The big challenge, however, is how to properly anonymize the data so that they can be shared securely with other institutions.
From Clinical Validation to Market Trust: Bayer’s Approach to AI in Radiology
This is a very dynamic time within the commercial realm of AI. Radiology, in particular, is one of the most mature fields in terms of a true marketplace. We are starting to see some winners and losers. How does a substantial company like Bayer navigate this fast, agile, and risk-loving landscape?
Dr. Seidensticker: Yes, it is indeed an area of cutting-edge science where we, like others, have to experiment and test new approaches for their validity. What we are seeing in the market is that although many AI tools are available in radiology, only very few are actually used and fully trusted. That means that there is a difference to pharma products in the sense that approved AI doesn't automatically mean it works perfectly everywhere. At this stage, people are increasingly looking for very specific AI solutions that clearly improve either the workflow or diagnostic accuracy in a distinct way. Providing that can be challenging. As a result, the most clinically valuable AI systems will likely have to undergo clinical trials similar to those required in pharmaceuticals. With our long-standing experience in clinical development and validation, we are well positioned to contribute meaningfully and responsibly to this evolving space. Bayer in Radiology for example offers a platform that is designed to support development teams in building new AI-enabled applications.
Do you see the implementation of AI as a second reader in screening protocols? Is that accelerating, slowing down, or staying relatively steady as it is being adopted in different types of screening processes?
Prof. Hamm: I definitely see it accelerating, for two main reasons. First, we will have more and more screening programs, such as breast cancer screening, lung cancer screening, and potentially others in the future, and there are simply not enough physicians. Ideally, screening should be double-read, but in the future, that may mean one physician and one AI system.
To put it simply, in screening programs like lung or breast cancer screening, the key question is just whether there is a lesion or not. This is something AI can answer effectively.
However, when you look at a patient who is ill and you perform a chest X-ray or CT, the findings can be much more complex. It could be cancer, inflammation, thromboembolism, or something else entirely. In such cases, AI might only recognize two out of five or six possible diagnoses. So, AI works well in screening where the question is binary — lesion or no lesion — but it cannot yet cover the full diagnostic spectrum.
Dr. Seidensticker: I fully agree with what Professor Hamm said. There is one interesting aspect regarding the use of AI as a second reader. The impact of AI can differ depending on whether it is used as a first or second read. For example, when AI is used as a first read, it can influence or bias the human reader’s attention because the interpretation is anchored on the AI’s suggestion.
In some studies, it has actually been shown that using AI as a second read — after the human reader — produces better outcomes than using it as the first read.